Ever wondered if a well-meaning rub could actually cause harm? You expect massage to ease pain and boost health, but pressure in the wrong spot can injure fragile structures just under the skin. Learn how to protect your body and confidence before you press down.
Some sites hide arteries, nerves, lymph nodes, or thin bone. Only a few places are truly off-limits, but many high-risk zones need light, diffuse touch or avoidance. This matters whether you use hands, tools, or help a family member at home in Turkey.
Throughout this guide you’ll get a clear safety framework: screen for risks, pick gentler pressure, and stop if sharp pain, tingling, or dizziness appears. For clinical contraindications and deeper detail, visit massage contraindications.
Key Takeaways
- You’ll learn exactly which areas to avoid or touch with extreme caution.
- Understand why neck, groin, behind-knee, armpit, abdomen, and low-back kidney zones are higher risk.
- Adopt a safety-first habit: stop when your body signals danger.
- Differentiate endangerment sites from true medical contraindications.
- Use lighter pressure and diffuse strokes when in doubt.
Massage safety first: areas of caution vs contraindications</h2>
Start every session by separating universal caution zones from client-specific contraindications. Endangerment sites are anatomical spots where vital structures lie close to the skin. If you press too deep or use a pinpoint tool, you risk injury.
What endangerment sites mean and why they matter
Endangerment sites are places where arteries, veins, nerves, lymph nodes, or thin bone sit shallow. These sites carry the same risk for everyone, so use lighter pressure and wide contact here.
Vulnerable structures you protect
- Arteries/veins: bleeding or clot risk if compressed.
- Nerves: slow to heal after direct trauma.
- Lymph nodes/vessels: delicate and superficial.
- Fragile bones: small processes and floating ribs risk fracture.
“Avoid digging with a thumb or elbow where you can feel a pulse.”
When to use light, diffuse pressure
Prefer palm-based effleurage and distributed contact over focused thumb or tool work. Broad techniques spread force across tissue and reduce compression against bone.
| Risk Type | Caution (endangerment sites) | Contraindications |
|---|---|---|
| Basis | Anatomy-based, applies to all clients | Medical condition or medication specific |
| Typical response | Use light, diffuse pressure | Modify or avoid therapy entirely |
| Examples | Carotid area, popliteal fossa, axilla | Blood thinners, acute infection, DVT |
Screen your health risks before you massage anything</h2>
A simple pre-session screen can protect you from complications and guide safe choices. Start by asking clear, brief questions about recent injuries, ongoing medications, and chronic conditions. This quick process keeps you in control of your health choices.
Absolute vs local vs relative contraindications
Absolute contraindications mean skip the session. Local contraindications ask you to avoid a single spot. Relative contraindications let you continue with modifications in pressure, time, or position.
Medication and medical condition check
Ask about blood thinners, diabetes, hypertension, and clotting disorders. Blood thinners raise bleeding risk and may call for very light touch. Uncontrolled hypertension or diabetes can make even light treatment unsafe without clearance.
Timing after injury: the first 48–72 hours
After a fresh injury, circulation increases and can worsen swelling or internal bleeding. Treat the first 48–72 hours as a no-massage window unless a clinician advises otherwise.
“When in doubt, modify—lighter pressure, shorter sessions, and safer regions protect recovery.”
| Check | What it means | Action |
|---|---|---|
| Recent trauma | Higher bleeding/swelling risk | Avoid for 48–72 hours |
| Blood thinners / clotting issues | Increased bruising, clot danger | Use light touch or seek clearance |
| Uncontrolled medical conditions | Unpredictable response to massage | Pause and get medical approval |
Use this short checklist before treatment. It helps therapists and clients make confident, safe choices while avoiding massage-related harm and promoting long-term health. For more practical tips, read a short guide on massage and stress relief in Kadıköy.
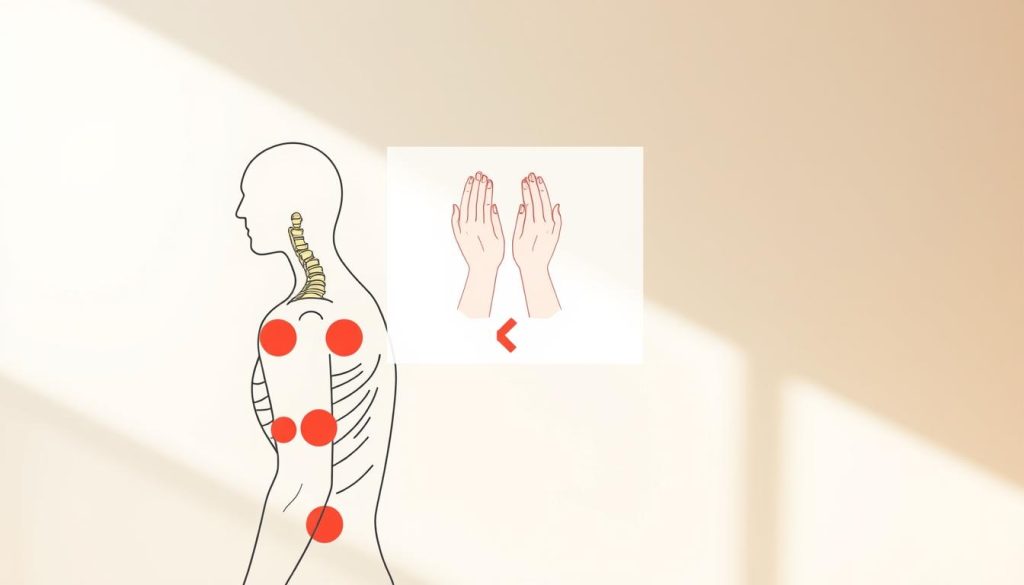
Which areas should not be massaged? The highest-risk body zones to avoid or treat with extreme caution</h2>
A few high-risk sites need light contact or total avoidance to protect blood flow and nerves.
Eyes and other truly off-limits tissues: never apply direct pressure to the eyeball or eyelids. These sites are delicate and can be damaged by even gentle force. Leave periocular work to trained clinicians and avoid any tool contact.
Front and sides of the neck: the anterior and lateral neck hide the carotid arteries, jugular vein, and vagus nerve. Firm pressure here can trigger dizziness, a sudden drop in blood pressure, or a slowed heart rate. Use only light, broad contact if you must work nearby.
Armpit and inner upper arm: the axilla contains major vessels, lymph nodes, and the brachial plexus. Deep, focused pressure can cause nerve pain, numbness, or vascular compression. For clients in Turkey or elsewhere, choose palm strokes and gentle holds.
Inner thigh and femoral triangle: the femoral artery, vein, and lymphatic tissue sit close to the surface. Deep thumbs or tools can raise the risk of bleeding, dislodging clots, or vein thrombosis. Avoid trigger-point digging in this region.
Back of the knee (popliteal fossa): bundled nerves and the popliteal vessels lie here. Never use deep compression or hard percussion behind the knee. Opt for light effleurage around the joint instead.
“If you work near vital structures, prioritize wide, gentle contact and stop at the first sharp pain, tingling, or dizziness.”
- Protect blood flow by reducing concentrated pressure near major veins and arteries.
- When in doubt, ask your client about clot history, recent surgery, or medications.
- Remember: light touch plus clear consent keeps therapy safe and effective.
Neck and head caution zones that can trigger dizziness, fainting, or nerve symptoms</h2>
Your neck and head need precise, gentle handling because small changes in pressure can cause big nervous-system responses.
Anterior cervical region and carotid sinus sensitivity
The carotid sinus near the bifurcation of the common carotid is a baroreceptor that helps regulate blood pressure. Firm, focused pressure here can trigger a sudden drop in blood pressure and fainting. When you work the front neck, use broad, light strokes and avoid direct compression of the sinus.
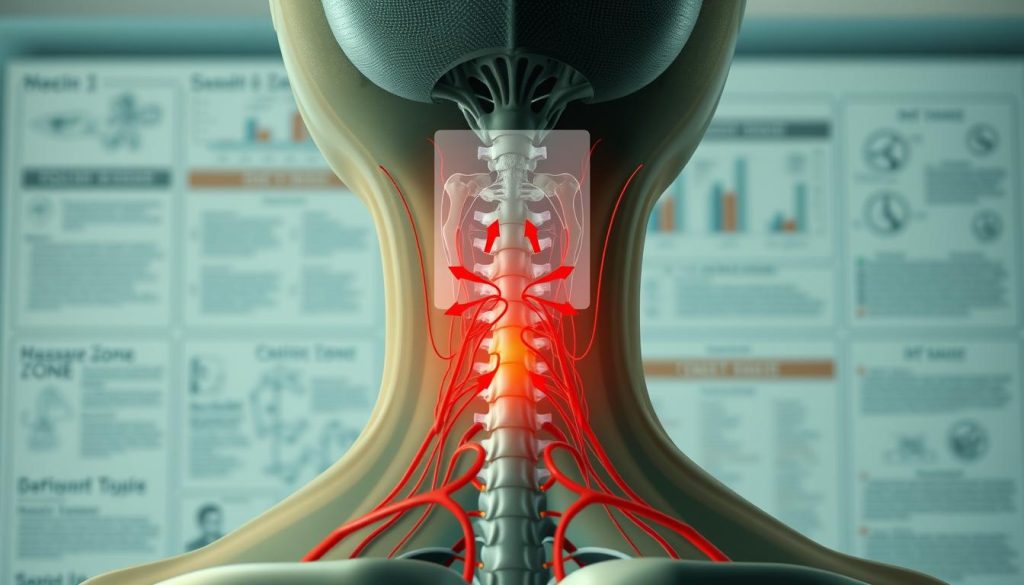
Posterior triangle and suboccipital area: why deep pressure can be risky
The posterior triangle holds the external jugular, subclavian vessels, and roots of the brachial plexus. Deep work can irritate nerves and disturb nearby vessels.
The suboccipital region contains occipital nerves and vertebral vessels. Excessive force here may cause nerve irritation, headache, or vascular symptom. Favor gentle, sustained contact and avoid sharp percussive moves.
Stop signals you should never push through: tingling, sharp pain, burning, or numbness
Red flags: tingling, numbness, burning, sharp or shooting pain, lightheadedness, or sudden nausea. These signs demand immediate pause.
“If your client reports tingling or sharp pain, stop, reassess, and switch to broader, softer techniques.”
| Zone | Main structures | Safe approach |
|---|---|---|
| Anterior neck | Carotid sinus, jugular vein | Light, broad effleurage; avoid direct compression |
| Posterior triangle | Brachial plexus roots, subclavian vessels | Avoid deep thumb work; use palm-based contact |
| Suboccipital area | Occipital nerves, vertebral vessels | Gentle holds, low pressure, short duration |
- You’ll treat the neck like a precision zone: small changes in pressure can alter nerve signals and blood pressure.
- Communicate constantly with clients and pause at any sign of unusual pain or tingling.
- When in doubt, choose wide contact and gentler techniques to protect health and prevent injury.
Abdomen and pelvis: where deep pressure can do real harm</h2>
Treat the belly with deliberate gentleness: deep force can harm organs hidden under thin tissue. You can offer soothing treatment here, but your priority is comfort and safety.
Umbilicus and organ-dense areas: work within comfort and avoid heavy pressure
The umbilicus hides vessels and multiple organs beneath a shallow layer of tissue. Use light, broad strokes and avoid digging or sustained focal pressure. If your client reports guarding, nausea, or sharp pain, stop immediately.
When enlarged or vulnerable organs raise risk: liver and spleen considerations
Enlarged liver or spleen from certain medical conditions increases bleeding and bruising risk. Never apply deep pressure over the upper-left or upper-right quadrants when those organs may be tender or swollen. Check medication and condition history first.
Pubic and urinary bladder region: technique and consent are non-negotiable
Consent matters: pelvic work requires clear permission and transparent boundaries. For pregnancy, avoid deep abdominal work and favor side-lying, gentle support. Scale your pressure to relax tissue, not to force it.
“When in doubt, choose gentle, sweeping strokes — your goal is comfort, not force.”
- You’ll learn to prioritize breath and relaxation over depth.
- Stop at any sign of guarding, sharp pain, or dizziness.
- For more on choosing the right technique, see a concise massage techniques guide.
Low back and kidneys: avoid percussion and heavy force</h2>
Treat the low back like a protected zone: gentle hands win over force every time. The kidney area on the posterior torso lies under thin soft tissue, so depth and impact can cause more harm than relief.
Why you must be cautious: kidneys are organs, not muscles. Deep pressure, tapotement, or mechanical percussion devices can increase the risk of injury and internal bruising.
Kidney region on the posterior torso: why deep work and tapotement are discouraged
Identify the flank and lower thoracic back as a “respect zone.” Heavy force does not equal better results here; it raises risks without improving function.
- Focus: aim your massage on paraspinal muscles and hip tissues, not directly over organs.
- Avoid: percussion, massage guns, or sharp tapping on the kidney line.
- Trust comfort: if pain feels deep or internal rather than muscular, lighten pressure and move away.
“Smart technique choices help you feel better without creating setbacks that stall healing.”
For deeper context on physiological effects, review a clinical overview at an expert chapter on organ-protective care. For practical tips and common challenges in massage practice, see a local troubleshooting guide at massage practice challenges and solutions.
Veins, blood clots, and blood pressure: when massage can become an emergency</h2>
When veins and blood pressure are unstable, a routine rub can turn dangerous fast.
Varicose veins and superficial veins have thin walls and faulty valves. Direct pressure can rupture tissue or dislodge a small clot. That can produce heavy bleeding or a clot that travels to the lungs.
Recognize DVT red flags: one-sided swelling, warmth, redness, and a deep aching pain in a leg are urgent signs. If you suspect a deep vein thrombosis, stop massage and seek immediate medical care. This is a medical emergency, not a tight muscle.
Blood thinners and high INR increase bruising risk and bleeding risk during treatment. When clients or you take anticoagulant medications, choose very light strokes, avoid deep friction, and document medical history before touching vascular zones.
“Never massage a known or suspected clot — dislodging it can lead to pulmonary embolism or stroke.”
- You’ll learn when massage crosses from helpful to hazardous; adjust pressure for blood pressure instability.
- Avoid direct work over varicose veins and ask about recent surgery, long travel, or clot history.
- When on blood thinners, favor gentle, short sessions and clear contraindications with a clinician when needed.
| Issue | Signs | Therapist action |
|---|---|---|
| Varicose veins | Visible bulging, tenderness, thin vessel walls | Avoid direct pressure; use light, surrounding effleurage |
| Suspected DVT | Unilateral swelling, warmth, redness, pain | Stop massage; urgent medical referral |
| On blood thinners / high INR | Easy bruising, prolonged bleeding | Use minimal pressure; get medical clearance for deep work |
Skin, inflammation, and infection: when touch spreads problems instead of relieving pain</h2>
When skin looks inflamed or an infection is active, gentle hands protect healing and the wider community.
Active bacterial, viral, and fungal infections require you to pause massage. Touch can move pathogens across skin and push them deeper into tissue. If a client has fever, spreading redness, or widespread symptoms, skip therapy until a clinician clears them.
Fragile skin and open wounds
Eczema or psoriasis flares, burns, and open lesions are local contraindications. When skin is cracked or weeping, friction can tear tissue and invite more infection.
Swollen lymph nodes and acute inflammation
Swollen nodes often signal your immune system is active. Avoid direct work on inflamed regions during acute illness. Gentle support around—but not over—the area is safer until swelling subsides.
“When infection is present, postpone, modify, or avoid massage so healing can proceed without added risk.”
- You’ll protect skin and others by delaying massage during contagious infections.
- Respect local contraindications like burns and open sores; return only with medical guidance.
- For a short recovery plan and practical tips, read this guide on massage for fatigue and recovery.
| Issue | Why it matters | Therapist action |
|---|---|---|
| Active infection | Risk of spreading pathogens; worsens inflammation | Postpone session; advise medical evaluation |
| Open wound / burn | Fragile tissue; high infection risk | Avoid area; follow wound-care guidance |
| Inflamed lymph nodes | Sign of systemic immune response | Avoid direct work; offer rest and hydration advice |
Conclusion</h2>
, Protect fragile anatomy with clear rules.
Keep this short checklist: eyes, front and side neck, axilla, inner thigh, and the back of the knee are high risk. Treat the abdomen and kidney line with gentle, broad contact only.
Understand the difference between anatomy-based caution and medical contraindications. When in doubt, choose light strokes and avoid focused, deep techniques.
Stop at once for tingling, numbness, burning, sharp pain, dizziness, or nausea. Respect the first 48–72 hours after injury as recovery time, not treatment time.
Seek help for suspected infection, clot signs, uncontrolled blood pressure, or unusual swelling. For a practical review of endangerment sites, read this concise guide: areas of caution in massage therapy.
Takeaway: the safest massage honors anatomy, your current health, and clear consent.